Press release: HKUMed researchers discovered that ORF8 and ORF3b are major targets of SARS-CoV-2 humoral immune response and can be used for more specific testing of COVID-19 infection
Researchers from HKU-Pasteur Research Pole at the School of Public Health, LKS Faculty of Medicine of The University of Hong Kong (HKUMed) used Luciferase Immunoprecipitation System (LIPS) assay and discovered that ORF8 and ORF3b are major targets of SARS-CoV-2 humoral immune response and can be used for more specific testing of COVID-19 infection. The study is the first among research teams worldwide to determine the most comprehensive “landscape” of antibody responses to SARS-CoV-2. The ground-breaking findings on COVID-19 serology are now published in Nature Immunology, a leading scientific journal.[link to the publication]
Antibody testing is an important tool in the response to COVID-19. It allows us to define the true extent of infection in the community, may help to confirm diagnosis in suspected patients and is needed for evaluation of vaccines. To date, SARS-CoV-2 antibody testing has been focussed on two proteins of the virus - the Spike protein as it correlates with neutralising capacity of the serum, and the Nucleocapsid protein as it is abundantly made by the virus and thus more likely to elicit detectable responses. Both proteins have potential problems with false positive reactions due to cross reactivity with antibody to other human coronaviruses which are common in the population.
The research team used the Luciferase Immunoprecipitation System (LIPS) assay, an antigen discovery tool previously used for screening cancer and new pathogen antigens, and assessed the antibody responses to 15 different SARS-CoV-2 proteins in 61 COVID-19 patients. They identified that two non-structural proteins, ORF8 and ORF3b, are key SARS-CoV-2 targets that elicit early and potent antibody responses in COVID-19 patients. These proteins are unique to SARS-CoV-2, thus are able to avoid the problem of cross-reactivity with other “common cold” human coronaviruses. Such robust antibody responses against these two viral proteins could be consistently detected in the majority of COVID-19 patients (96.5% sensitivity).
Currently, ORF3b and ORF8 proteins are not mainstream targets for COVID-19 diagnosis. These findings will improve the serological tests for COVID-19 and enhance the development of second-generation diagnostic tests.
About the research team
The research was conducted by a team led by Dr Sophie Valkenburg, Research Assistant Professor, HKU-Pasteur Research Pole (HKU-PRP), School of Public Health, HKUMed. Other members of the research team from HKU-PRP included Ms Asmaa Hachim, Research Assistant; Ms Carolyn A Cohen, PhD student; and Dr Niloufar Kavian-Tessler, Post-doctoral Fellow and Honorary Visiting Fellow from Paris Descartes University and Cochin Hospital (France). Members from the School of Public Health, HKUMed included Dr Alex Chin Wing-hong, Investigator; Dr Daniel Chu Ka-wing, Research Assistant Professor; Dr Chris Mok Ka-pun, Research Assistant Professor; Dr Ranawaka APM Perera, Research Assistant Professor; Professor Leo Poon Lit-man, Professor and Head of Division of Public Health Laboratory Sciences; and Professor Malik Peiris, Tam Wah-Ching Professor in Medical Science and Chair Professor of Virology. Members from Princess Margaret Hospital were Dr Owen Tsang Tak-yin, Medical Director, Hospital Authority Infectious Disease Centre; and Dr Yeung Yiu-cheong, Specialist in Respiratory Medicine.
This project was supported by the Health and Medical Research Fund (Ref: COVID-190115), Food and Health Bureau, and General Research Fund (Ref: 17113718), Research Grants Council,Government of Hong Kong Special Administrative Region.
About HKU-Pasteur Research Pole
HKU-Pasteur Research Pole (HKU-PRP) is a joint laboratory of HKU and Institute Pasteur, co-directed by Professor Roberto Bruzzone and Professor Leo Poon Lit-man, established in 2000 with the aim to developing programmes of excellence in research and education that will generate biological knowledge and advance the understanding and treatment of infectious diseases. HKU-PRP benefits from the outstanding scientific environment offered by the School of Public Health of the LKS Faculty of Medicine, with its significant contributions, both locally and internationally, to research on emerging viral diseases and improving health. Moreover, HKU-PRP is part of the IP International Network, a unique model for health cooperation to further science, medicine and public health with more than 100 years of history.
http://www.hkupasteur.hku.hk
About the School of Public Health, HKUMed
The School of Public Health, LKS Faculty of Medicine of The University of Hong Kong has a long and distinguished history in public health education and high impact research. With world leading research in infectious diseases as well as on non-communicable diseases of both local and global importance, the School has made significant contributions through its research and advocacy to improve the health of populations and individuals, both locally and globally. The School is a leading research and teaching hub in public health on influenza and other emerging viruses, control of non-communicable and infectious diseases, tobacco control, air pollution, psycho-oncology, behavioural sciences, exercise science, life-course epidemiology, and health economics, health services planning and management. This work has informed international (e.g. the US Food and Drug Administration, Health Canada, the World Health Organization), national and local public health policies.
For the latest update from HKUMed on COVID-19:
http://www.med.hku.hk/en/covid-19

Researchers at HKU Pasteur Research Pole, School of Public Health, LKS Faculty of Medicine at The University of Hong Kong (HKUMed) used Luciferase Immunoprecipitation System (LIPS) assay and discovered that ORF8 and ORF3b are major targets of SARS-CoV-2 humoral immune response and can be used for more specific testing of COVID-19 infection.
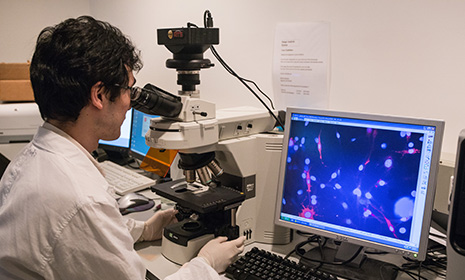
Blood from COVID-19 patients contains antibodies early after infection, that bind ORF3b and ORF8 proteins. These antibodies were detected by proteins tagged with fluorescent labels by LIPS. As these proteins are unique to the SARS-CoV-2 virus, antibodies from uninfected people would not bind these targets. Thus, LIPS is able to demonstrate a significant difference in antibodies between COVID-19 patients and uninfected (negative) people. (Figure: generated by Biorender)







.png)
